Kalderos Launches Review, an Enhanced 340B Claims Verification Platform
Review is a culmination of feedback and continued collaboration with covered entity partners
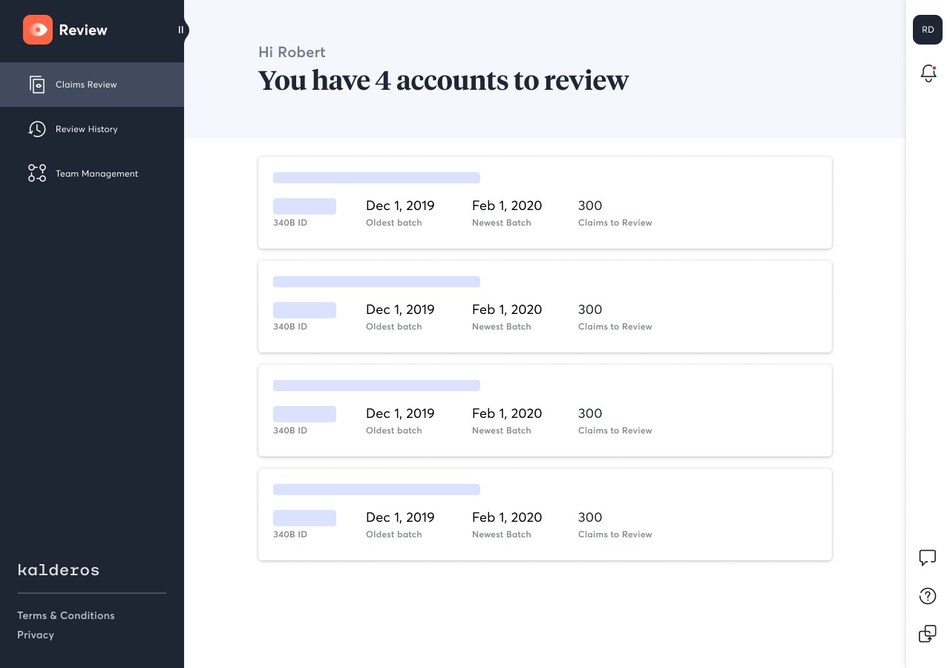
Kalderos, the creator of the country’s first and only drug discount management solution, announced the launch of its enhanced and streamlined covered entity-facing platform, Review. Review builds on the company’s legacy claims verification software for covered entities, with updates to create a more intuitive, efficient and accurate 340B claims verification process.
“At Kalderos, we’re building an intelligent infrastructure that supports the 340B Program and provides clarity for all stakeholders,” said Jeremy Docken, CEO and co-founder, Kalderos. “Every 340B stakeholder is working toward the shared goal of ensuring the program works on behalf of patients. Review will enable our covered entity partners to spend less energy on verifying claims and more time where it matters most: providing lifesaving care.”
Recommended AI News: Telecom Argentina Transforms Technology, Culture and Processes to Deliver First Quad-Play Bundle in Latin America
Retiring the previous brand name, Grappa, the latest upgrades to the covered entity-facing platform include:
- Enhanced algorithm precision: With investments to its data science team, Kalderos has built upon its industry-leading algorithm for increased accuracy.
- Simplified review process: Streamlining the claims review process, Review provides a more comprehensive view of claims data, including Medicaid agency and plan type. Additionally, Review incorporates a wider range of response options to allow users to provide more feedback when a simple “yes” or “no” answer isn’t sufficient.
- Enable teamwork: Collaboration — within a covered entity’s team and out — is crucial to ensure 340B compliance. As a result, Review now supports multiple users per 340B ID so responses can be provided by more than just one authorized user.
- Respond using a preferred format: Augmenting Review’s updated and simplified user interface, Review offers users more options to respond to claims, allowing covered entities to use their preferred format. Users can now upload Excel and CSV files.
Recommended AI News: Car Rental Platform EasyRentCars Evolves its Brand to QEEQ for More Travel Services and Daily Savings
“In bringing Review to fruition, we emphasized feedback sessions and beta testing with our covered entity partners to understand what additions would support them in their work,” said Steve Zielinski, Director of Industry Relations, Kalderos. “Collaboration is part and parcel to 340B Program integrity and we’re proud to be a continued partner with thousands of covered entities.”
Following the recent updates, 340B consulting group Advis said, “The new user interface enables us to comprehensively review 340B claims on behalf of our covered entity clients. Expanded response types, paired with broadened export capabilities, enhance efficiency and accuracy as we work with hospitals to demonstrate their compliance with all 340BProgram rules.”
Founded in Chicago in 2016, Kalderos is committed to building a drug discount management solution that supports accurate discount effectuation, ensuring the right discount goes to the right party on the right transaction.

Comments are closed, but trackbacks and pingbacks are open.